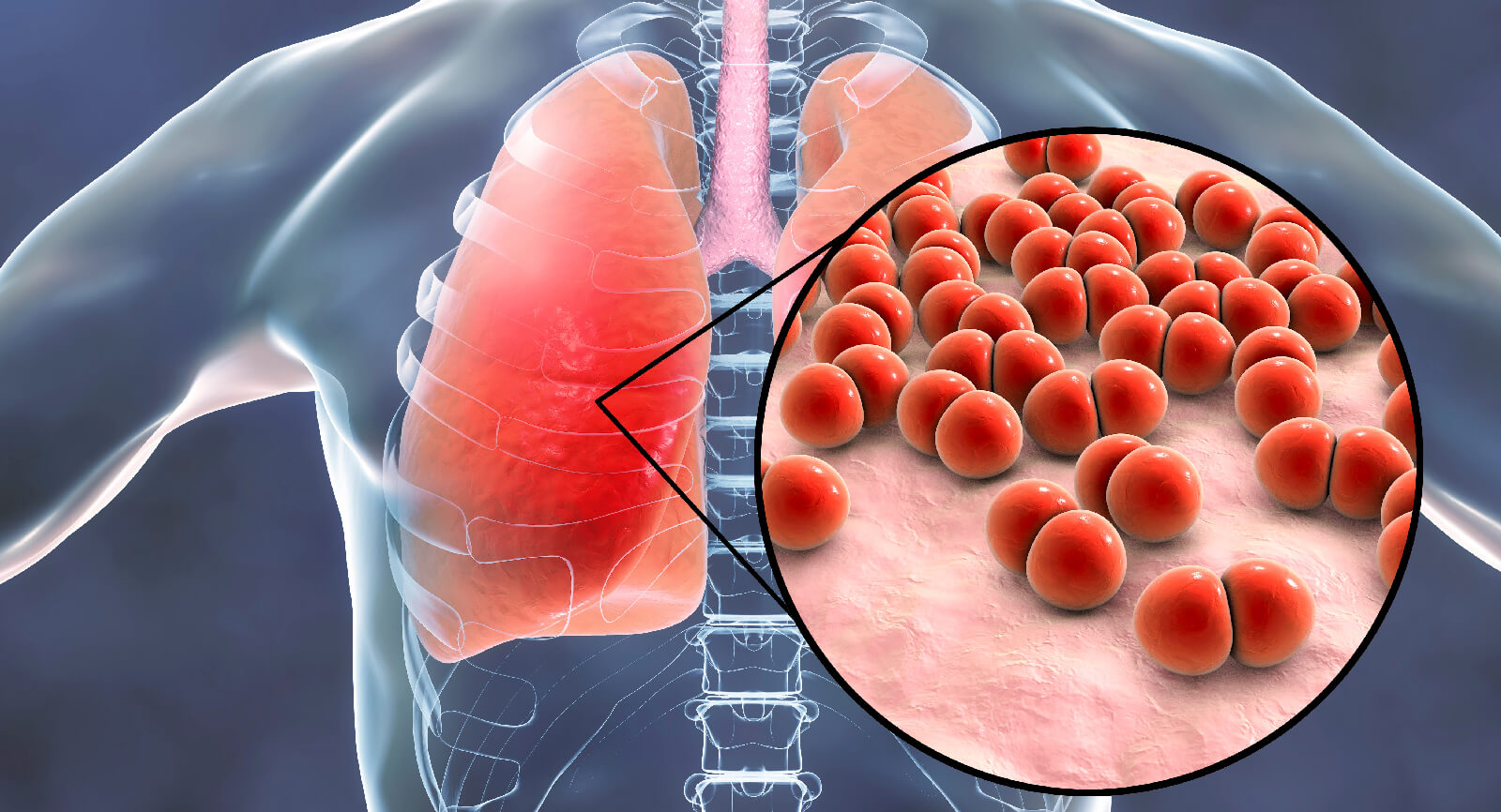
India has 18% of the global population and an increasing burden of chronic respiratory diseases1. The technique of nebulisation is commonly utilised in the treatment of such diseases including asthma, cystic fibrosis and chronic obstructive pulmonary disease (COPD)2. Recent improvements in nebuliser technologies have led to the development of vibrating mesh nebulisers (VMNs) that produce a consistent and improved aerosol generation efficiency and low residual drug volume2. The Aerogen Solo and Pro utilise VMN technology. The nebulisers are comprised of a unique dome-shaped aperture plate containing approximately 1,000 precision-formed tapered holes, surrounded by a vibrational element. When energy is applied, the aperture plate vibrates at 128,000 times per second. Each one of the 1000 cone-shaped apertures within the mesh acts as a micropump drawing liquid through the holes producing a low velocity aerosol optimised for targeted drug delivery to the lungs2,3. Each aperture creates particles of 1-5 µm in diameter, which is the optimum particle size for efficient lung deposition. Particles larger than 10–15 µm are deposited in the nose and mouth; particles that are 5–10 µm in size tend to deposit in the upper airways, while particles sized 1–5 µm have a greater probability of reaching the lower respiratory tract (i.e. from the trachea to the lung periphery)4.
The Aerogen Solo has an in-line circuit design, so the ventilator circuit does not need to be disconnected for drug delivery. It is designed so that the medication reservoir is isolated from the breathing circuit minimising the potential for nebulisation of contaminated fluids and delivers the medication dose with minimal residual remaining after nebulisation5. In addition, the Aerogen Solo is virtually silent in operation (<35 dB measured at 0.3 metre distance)5. Unlike ultrasonic nebulisers (USNs), Aerogen technology does not increase the drug solution temperature as there is no heat generated during use6. During mechanical ventilation (MV) with active humidification, the nebuliser can be placed on the dry side of the humidifier or at the inspiratory limb of the breathing circuit before the patient wye. The Aerogen Solo can also be placed on the patient side of the wye and this facilitates the use of a Heat and Moisture Exchanger; however, this placement is contraindicated for neonates5. During non-invasive ventilation (NIV), the Aerogen Solo can be used in the same positions with a dual limb circuit. The Aerogen Solo may be utilised with single limb NIV circuits using non vented masks, with the nebuliser placed between the exhalation port and the patient5.
Several studies have demonstrated optimal aerosol delivery with Aerogen VMN technology compared with jet nebulisers (JNs) and USNs in the critical care environment7–10. Ari et al. demonstrated improved inhaled dose with the Aerogen Solo compared with JN when placed before the humidifier compared to placement at the wye with both adult and paediatric MV models with bias flow9. Improved aerosol delivery with VMN technology is also associated with the minimal residual volume left in the device at the end of the treatment. Standard JNs leave up to 2 mL of the drug behind which can also be costly when using expensive drugs11,12. Dugernier et al. compared lung deposition with radiolabelled aerosol delivered via VMN in two modes of ventilation, pressure support (PSV) and volume-controlled ventilation (VCV) in a randomised controlled trial of neurosurgical patients with healthy lungs. They demonstrated 10 % and 15 % lung dose with PSV vs VCV, respectively7. Macintyre et al. previously administered radiolabelled aerosol with a JN to MV patients and they showed 2.9% lung deposition8. In comparison with the MacIntyre study, the Dugernier study demonstrated greater lung deposition with the VMN regardless of the mode of ventilation7,8.

In a recent review, Ari reported practical strategies for safe and effective aerosol delivery of aerosolised medications to ventilated patients with COVID-19. Delivering aerosolised medications via JN or pMDIs was deemed not to be appropriate due to the breakage of the circuits for the placement of the device on the ventilator circuit before aerosol therapy13. The benefits of VMN technology were highlighted including the fact that VMNs can stay in-line for up to 28 days as well as the reservoir design that allows addition of medication without requiring the ventilator circuit to be broken for aerosol drug delivery. Furthermore, this review article recommended to place the VMN at the dry side of the humidifier to improve the efficiency of the treatment and further reduce retrograde contamination from the patient13. Similarly, Dhand and Li outlined the suitability for use of VMN technology in the context of COVID-19. The authors reported that VMNs generate aerosols via mesh plates that separate the sealed medication reservoir from the patient interface, the aerosol derives from the fluid in the nebuliser chamber and does not carry patient-derived viral particles14. In contrast, residual drug remaining in JNs or USNs at the end of treatment could act as a breeding environment for bacteria if the nebuliser remains in the circuit between treatments14. In a letter to the editor of the Journal of Critical Care, Miller et al. reported safe and efficient bronchodilator administration using continuous nebulisation with the Aerogen Solo in invasively and non-invasively ventilated COVID-19 patients with COPD and asthma, and highlighted that the closed system requires minimal staff handling and no circuit opening, thereby reducing workload and increasing safety15. This is the first report of administering bronchodilators safely and efficiently to COVID-19 ventilated patients15. An expert consensus on reducing viral transmission during respiratory care for patients infected with COVID-19 has recommended to use a VMN for mechanically ventilated patients COVID-19 patients requiring inhalation therapy16. The consensus discussed how an additional filter should be placed at the expiratory port of the ventilator during nebulisation and the VMN should be positioned at the dry side of the humidifier16. In a consensus document on NIV support for adult patients with acute respiratory failure secondary to SARS-CoV-2 infection, a circuit with a VMN elbow was recommended as first choice when using inhaled therapy with NIV.
Note: This editorial was produced and sponsored by Aerogen and compiled by Millind Mahajan , Regional Sales Manager – West
PM749
If you would like to receive additional information on Aerogen or arrange for a free virtual product demonstration, please contact us below;
Rajiv Julka, Country Manager – India & Sub-Continent
Kamal Kishore, Business Manager
Aerogen Medical Devices India Pvt. Ltd.
131, ABW Rectangle One Building,
D-4, Saket District Centre, New Delhi,
India – 110017
Office: +91 11 41422577
Email: [email protected] ; [email protected] ; [email protected]
References
1. Salvi S, Anil Kumar G, Dhaliwal RS, Paulson K, Agrawal A, Koul PA et al. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Heal 2018; 6: e1363–e1374.
2.Ari A. Jet, Ultrasonic, and Mesh Nebulizers: An Evaluation of Nebulizers for Better Clinical Outcomes. Eurasian J Pulmonol 2014; 16: 1–7.
3 .Vecellio L. The mesh nebuliser: a recent technical innovation for aerosol delivery. Breathe 2006; 2: 252–260.
4.McNulty W, Usmani OS. Techniques of assessing small airways dysfunction. Eur Clin Respir J 2014; 1. doi:10.3402/ECRJ.V1.25898.
5 .Aerogen Solo System Instruction Manual. Aerogen Ltd. P/N 30-354, Part No. AG-AS3050. .
6 .Sidler-Moix A-LL, Di Paolo ER, Dolci U, Berger-Gryllaki M, Cotting J, Pannatier A. Physicochemical aspects and efficiency of albuterol nebulization: comparison of three aerosol types in an in vitro pediatric model. Respir Care 2015; 60: 38–46.
7.Dugernier J, Reychler G, Wittebole X, Roeseler J, Depoortere V, Sottiaux T et al. Aerosol delivery with two ventilation modes during mechanical ventilation: a randomized study. Ann Intensive Care 2016; 6: 73.
8 .MacIntyre NR, Silver RM, Miller CW, Schuler F, Coleman RE. Aerosol delivery in intubated, mechanically ventilated patients. Crit Care Med 1985; 13: 81–84.
9.Ari A, Atalay OT, Harwood R, Sheard MM, Aljamhan EA, Fink JB. Influence of nebulizer type, position, and bias flow on aerosol drug delivery in simulated pediatric and adult lung models during mechanical ventilation. Respir Care 2010; 55: 845–851.
10.Ari A, Areabi H, Fink JB, Cpft PT, Areabi H, Rrt M et al. Evaluation of aerosol generator devices at 3 locations in humidified and non-humidified circuits during adult mechanical ventilation. Respir Care 2010; 55: 837–844.
11.Gardenshire, DS. Burnett, D. Strickland, S. Myers T. A Guide To Aerosol Delivery Devices for Respiratory Therapists. https://www.aarc.org/wp-content/uploads/2015/04/aerosol_guide_rt.pdf. 2017.
12.Ari A, Fink JB, Dhand R. Inhalation Therapy in Patients Receiving Mechanical Ventilation: An Update. J Aerosol Med Pulm Drug Deliv 2012. doi:10.1089/jamp.2011.0936.
13 .Ari A. Practical strategies for a safe and effective delivery of aerosolized medications to patients with COVID-19. Respir Med 2020; 167: 105987.
14.Dhand R, Li J. Coughs and Sneezes: Their Role in Transmission of Respiratory Viral Infections, Including SARS-CoV-2. Am J Respir Crit Care Med 2020. doi:10.1164/rccm.202004-1263PP.
15.Miller A, Epstein D. Safe bronchodilator treatment in mechanically ventilated COVID-19 patients: A single center experience. J. Crit. Care. 2020; 58: 56–57.
16.Respiratory care committee of Chinese Thoracic Society. [Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia]. Zhonghua Jie He He Hu Xi Za Zhi 2020; 17: E020.