In the current healthcare reality, decisions based on diagnostics set the course for the entire patient journey prior to any treatment. As healthcare challenges become more intricate, patients become more complex, expectations rise, and healthcare systems become more time constrained, the focus has shifted to completion of the right tests, optimally timed.
In the year 2026, diagnostic precision is no longer solely a lab value. It is a clinical value that integrates technology, time, and a thoughtful approach to decision making in order to improve outcomes and elevate confidence in the healthcare process.
In modern healthcare, diagnostic precision is no longer a function of technology, but rather, time, context, and clinical relevance. In 2026, the emphasis on diagnostics is no longer on volume, but on the right test completed at the right time.
In doing so, healthcare has entered a new frontier in diagnostics.
From a Volume to Value Approach
Traditionally, a measure of success in diagnostics was the sheer volume of tests undertaken. Equally, unconstructive provisioning of poor tests that fall outside of the scopes of time could lead to significant delays in patient care and increased costs.
The focus of value-based diagnostics includes:
- Selection of tests based on data
- Relevance of tests to the clinical situation as opposed to redundancy of tests
- Shorter diagnostic processes
- More certainty in diagnosis
Healthcare systems are managing costs and improving value by optimizing diagnostic plans to the symptoms, stage of the disease, and risk factors of the patient.
Clinical Decision Support and Smart Test Selection
By 2026, diagnostic precision is significantly enhanced by Clinical Decision Support Systems (CDSS) that are embedded in the hospital information systems. These systems assist clinicians in choosing the most appropriate tests based on the patient’s history, symptoms and clinical guidelines.
AI-based systems are assisting in:
- Providing recommendations on the most appropriate test panels
- Reducing unnecessary testing and testing of low value
- Identifying and reporting important findings in real time
- Helping in the active surveillance of diseases
This smart use of tools is designed to improve clinical diagnostics rather than the other way around.
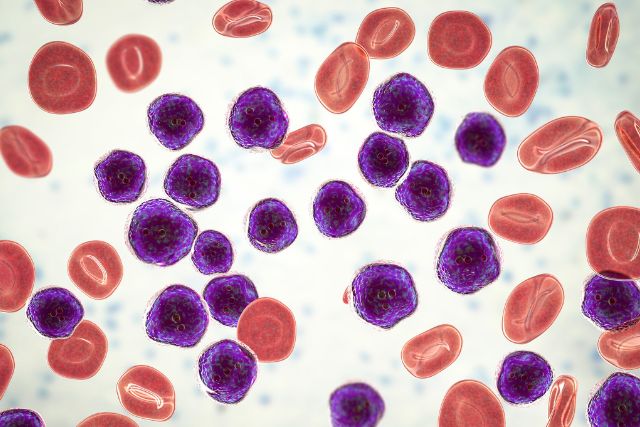
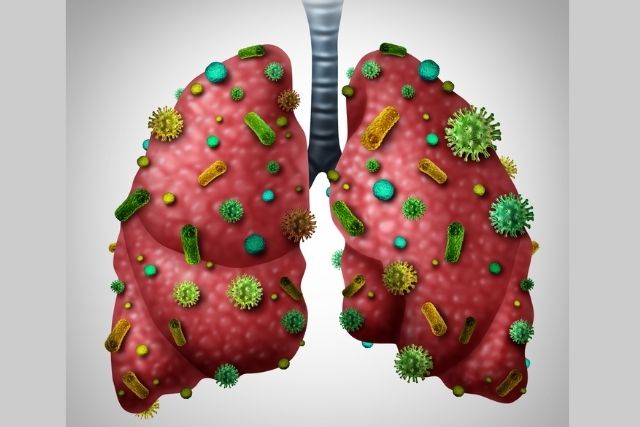
Speed Without Compromise: the Role of Rapid Diagnostics
In certain areas of care such as emergency medicine, infectious disease, oncology, and critical care, life-saving diagnosis can and must be done swiftly. Rapid diagnostic tools are revolutionizing the way healthcare is provided. They are capable of offering more and more accurate answers in shorter time intervals.
Noteworthy improvements encompass:
- POCT for more rapid clinical determination
- Targeted rapid molecular analyses for infectious diseases
- Rapid high throughput analyzers for emergent clinical laboratories
- Real-time data integration with electronic medical records
The aforementioned factors have now resulted in clinical decision support systems to provide more rapid clinical interventions, optimize length of stay in the hospital, and achieve better outcomes for patients—all without sacrificing analytical precision.
Diagnostics and Personalization of Care
The tenet of the “right test” is intimately aligned with personalized medicine. Developments in genomic, proteomic, and molecular diagnostic sciences have enabled clinicians to optimize testing approaches to the specifics of the patient.
In the clinical management of oncology, rare diseases, and chronic disease, precision diagnostics permit:
- structuring disease stratification early and accurately,
- selection of targeted therapies,
- monitoring of responsiveness to therapies,
- reduction of trial and error.
This personalized diagnostic framework is designed to ensure that every test provides clinically relevant information.
The Elimination of Diagnostic Error Through Integration and Quality The gaps in diagnostics have resulted from fragmented data, delayed data reporting, and a lack of effective communication among the clinical and laboratory staff.
Integrated laboratory systems for the year 2026 have employed the following to reduce gaps:
- repetitive and unchanged methods in laboratory testing
- automation in the control and validation of laboratory procedures
- differentiated and compatible systems for hospitals and laboratories
- Distributed and integrated systems for continuous monitoring of system performance
The systems of accreditation and digital quality management have strengthened the gaps in reliability and compliance in the diagnostics workflows.
Patient-Centric Diagnostics: Transparency and Trust Repairs
Today’s patients are more educated and involved in their own healthcare. Trust is gained with clear and timely diagnostics and improves adherence to treatment plans.
Today’s diagnostic services focus on:
- Quicker delivery of reports
- More streamlined and understandable results
- Digital access via patient portals
- Lower rates of duplicate testing
By placing patients at the centre of diagnostic pathways, healthcare providers strengthen confidence and care continuity.
The Road Ahead
“Right Test, Right Time” is more than a diagnostic slogan—it is a strategic philosophy shaping the future of healthcare. In 2026, diagnostic accuracy is defined by intelligent test selection, timely execution, and meaningful clinical impact. As healthcare systems move toward value-based care models, diagnostics will continue to play a pivotal role in delivering precise, efficient, and patient-focused outcomes. The future of healthcare lies not in more tests—but in smarter diagnostics that truly make a difference.